What Church Leaders Should Know about Monkeypox
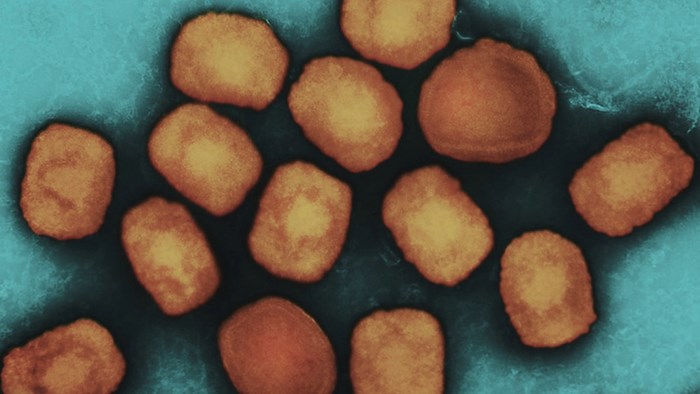
Monkeypox continues to spread across the United States and around the globe--but is your church ready?
To help you and your church better prepare and care amidst this public health emergency, we recently interviewed Rev. Dr. Que English. Below is part two of our conversation with her on what churches need to know about monkeypox prevention. In case you missed part one of our interview, you can find it here.

Dr. Que English
Rev. Dr. Que English serves as the Director of the Center for Faith-Based and Neighborhood Partnerships at the U.S. Department and Health and Human Services (HHS). In this role, she works closely with the White House Office of Faith-based and Neighborhood Partnerships, along with the CDC and offices like the Administration for Children and Families. The HHS Center’s core focus areas include addressing COVID-19, maternal health, mental health in youth, suicide prevention, and overdose prevention.
JA: What sort of precautions can churches take to reduce the risk of monkeypox?
QE: While human-to-human transmission of monkeypox virus primarily occurs by direct contact, it can also be transmitted during prolonged face-to-face contact.
If a monkeypox case has been identified in the community, consider the following actions:
- Communicate with staff and community members. Provide clear information to them about monkeypox prevention, including the potential for transmission through close and sustained physical contact, including sexual activity.
- Keep messages fact-based to avoid introducing stigma when communicating about monkeypox.
- Isolate staff or community members who have monkeypox away from congregate settings until they are fully recovered. A person is considered infectious until there is full healing of the rash with formation of a fresh layer of skin. Flexible, non-punitive sick leave policies for staff members are critical to prevent spread of monkeypox.
- Ensure access to handwashing. Soap and water or hand sanitizer with at least 60% alcohol should be always available. Anyone who touches lesions or clothing, linens, or surfaces that may have had contact with lesions should wash their hands immediately.
- Clean and disinfect the areas where people with monkeypox spent time and avoid activities that could spread dried material from lesions (e.g., use of fans, dry dusting, sweeping, or vacuuming) in these areas. Perform disinfection using an EPA-registered disinfectant with an Emerging Viral Pathogens claim, which may be found on EPA’s List Q, and follow the manufacturer’s directions.
- Provide appropriate personal protective equipment (PPE) for staff and community members who are in direct contact with people with known or suspected monkeypox infection. Also, provide PPE for those cleaning and disinfecting areas where people with monkeypox spent time.
KA: What about vaccines for preventing the monkeypox virus?
QE: The preferred vaccine to protect against monkeypox is JYNNEOS, which is a two-dose vaccine. Protection conferred by the JYNNEOS vaccine requires two doses given 28 days apart. It takes 14 days after getting the second dose of JYNNEOS for its immune protection to reach its maximum effectiveness.
The ACAM2000 vaccine may be an alternative to JYNNEOS. ACAM2000 is a single-dose vaccine, and it takes four weeks after vaccination for its immune protection to reach its maximum effectiveness. However, it has the potential for more side effects and adverse events than JYNNEOS. It is not recommended for people with severely weakened immune systems and several other conditions.
On August 15, HHS announced up to 442,000 doses of the JYNNEOS vaccine are now available for states and jurisdictions to order under an accelerated Phase 3 of the National Vaccine Strategy (NVS) to combat the current monkeypox outbreak.
JA: How might churches who want to address monkeypox in their communities get more involved?
QE: There are several ways to help:
- Promote messaging that provides information on what monkeypox is, how it can spread, and encourage those experiencing monkeypox-like symptoms to seek health care.
- Emphasize that anyone can get monkeypox and promote it as a public health concern for all. Focusing on cases among gay and bisexual men may inadvertently stigmatize this population and create a false sense of safety among those who are not gay and bisexual men.
- Invite local health experts to educate your community on the monkeypox virus, how to prevent it, and how to prevent it from spreading to others.
- When using images of the rash from patients with monkeypox, focus on how cases typically appear in the current outbreak and avoid showing extreme cases, unless necessary.
- Include pictures of people from diverse backgrounds and racial/ethnic groups.
KA: Where can church leaders turn for accurate and trusted information on monkeypox?
QE: Information and resources provided by the Centers of Disease Control and Prevention (CDC) is your community’s go-to place to learn about monkeypox and how to prevent the virus from spreading in your community.
Also visit the 2022 U.S. Map & Case Count to track the cases around the U.S.
JA: Is there anything else you think would be helpful for churches to know about monkeypox?
QE: As of August 15, 11,177 monkeypox cases have been reported in the United States—and you can check for updates here.
HHS is aggressively responding to the outbreak, and preventing spread of the monkeypox virus is a critical priority for HHS. We have launched a rapid and comprehensive response, significantly increased vaccine supply and distribution, expanded access to tests, made treatments available for free, and are educating the public on steps to reduce risk of infection.
However, we need the assistance of every faith leader in every community to provide accurate information to their community members so they can make informed decisions and stop the spread of the virus.
Jamie Aten, Ph.D. and Kent Annan, M.Div. co-direct the Humanitarian Disaster Institute at Wheaton College and are also the co-founders of Spiritual First Aid.
The Better Samaritan is a part of CT's
Blog Forum. Support the work of CT.
Subscribe and get one year free.
The views of the blogger do not necessarily reflect those of Christianity Today.