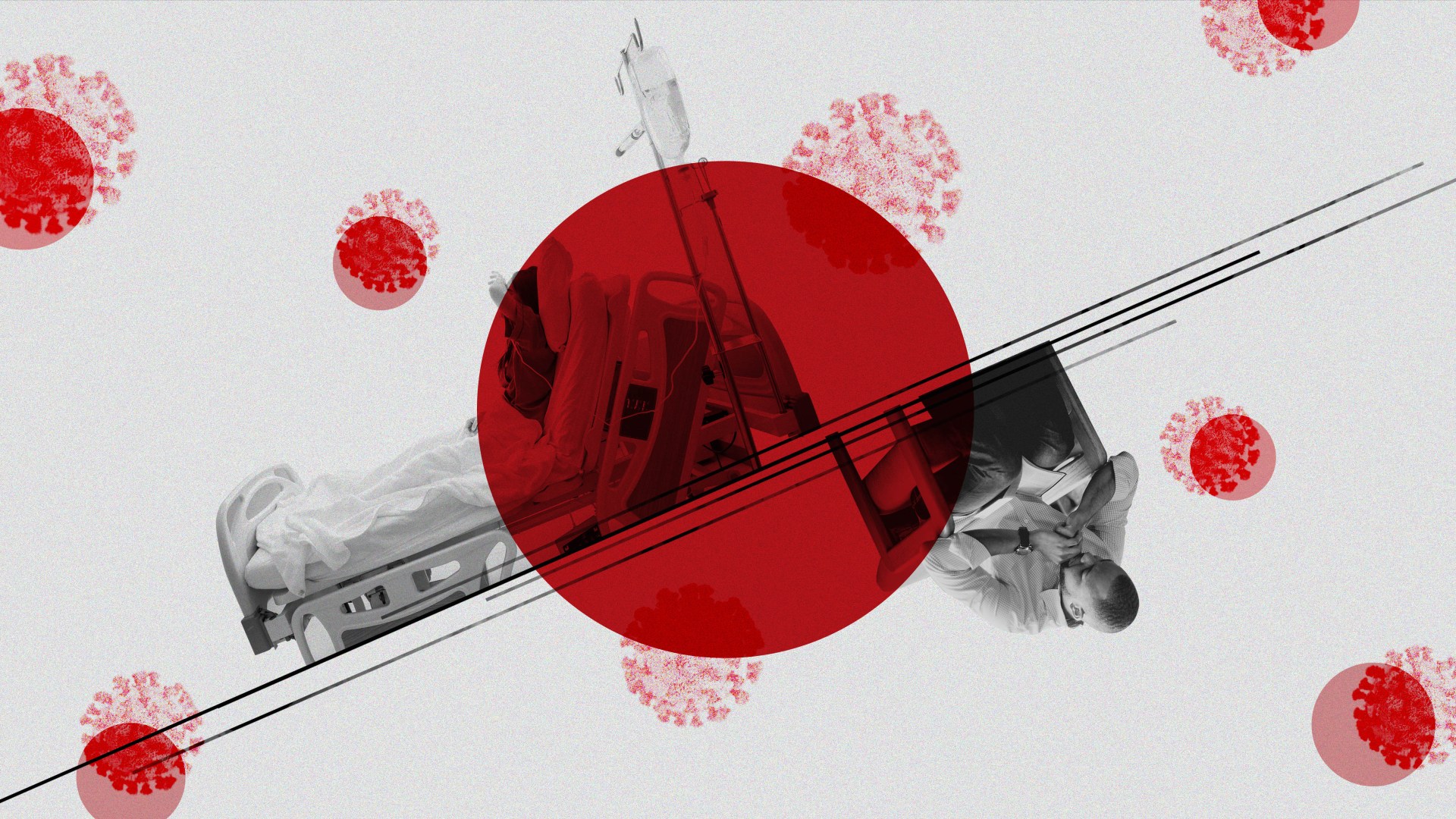
As medical facilities restrict visitors and ration protective gear amid the coronavirus pandemic, more hospital chaplains have been forced to do their job at a distance, while ministering to an onslaught of weary patients, families, and health care staff.
“Due to supply shortages of masks, this means that isolation rooms may involve phone calls, notes, letters, a wave through the door rather than (a chaplain being) inside the room,” said Heidi Greider, manager of spiritual care at Seattle Children’s Hospital.
Though individual institutions ultimately determine their own policies, guidelines from the Centers for Disease Control and Prevention play a factor. CDC guidance issued in February urged facilities to limit visitors, and as the outbreak has worsened, hospitals with COVID-19 patients have continued to tighten restrictions, including on chaplains.
Tim Kinnersley, lead chaplain at Northside Hospital Cherokee in Canton, Georgia, just got word this week that his hospital put a hold on all in-person chaplain visits to reduce the number of potential carriers coming in and out of the facility.
His case is not an anomaly. Another chaplain recalled how over two weeks her hospital went from allowing any guests to only permitting visits in end-of-life situations. In some cases, even medical staff are limited to one or two per room when the patient is known to be infected.
As the pandemic spread, CT heard reports of chaplains losing access to facilities—hospitals, hospices, nursing homes, and prisons—across the country, including in New York, Massachusetts, Illinois, Florida, Texas, and Kansas.
COVID-19 represents an unprecedented burden on the health care system and patients themselves, often isolated from family members and left wondering about their fate as researchers try to better understand the new disease.
“My chaplains know that a big part of their calling in this time is to be present and encourage everyone they encounter,” said Greider in Seattle, an early epicenter for coronavirus in the US. “Their calm demeanor, smiles, and even laughter are needed in this time.” Whether or not they are allowed to minister bedside, chaplains are in demand more than ever.
Chaplains are used to fast-paced, high-stress environments in trauma bays and emergency rooms, and some chaplaincy programs even use mock pandemic scenarios as practice. From the start of the COVID-19 outbreak in the United States, chaplains have sat on task forces assembled to address the virus.
“Chaplains are trained health care professionals,” Brent Bond, senior director of chaplaincy for the North American Mission Board (NAMB), told CT on Friday. “Many have gone through extensive training to be prepared for situations like this.”
Staying bedside
In some health networks, chaplains are considered essential members of the care team and encouraged to keep interacting face to face (or mask to mask). Chaplains are enlisted to meet with patients all the way from admissions rooms to emergency rooms and surgery wards.
But under the current restrictions on guests, most chaplains will have to wait for explicit invitations to enter a hospital room, if they are allowed in at all, rather than making the rounds and visiting room by room.
Like other health care workers, chaplains wear extra protective gear, including masks and gloves, even to visit non-COVID-19 patients, in order to reduce the risk of exposure. Chaplains seeing infected patients in-person need to take extra sanitizing precautions and keep their visits short.
Because patients are restricted from seeing family and friends, the chaplains who are able and willing to visit are playing an even more crucial role providing comfort and company.
“The fact that the chaplain is there to listen and to attend to the patients is actually something we’re seeing that’s invaluable to the holistic care of the patients,” said Doug Carver, a retired Army chaplain and executive director for chaplaincy for NAMB, where he helps lead more than 3,700 Southern Baptist chaplains.
With 728 deaths in the US as of Wednesday, and more patients being put on life support, the worst-case fear for many hospitalized due to the virus is that they would end up dying alone there.
“For end-of-life situations, the chaplains in many of these institutions are still allowed to provide that ‘ministry of presence’ at the time of death or transition,” said Bond. “I think that is continuing in most of the hospitals.”
Chaplains are engaging in more life-and-death discussions overall, as the reality of death becomes more immediate.
“Our chaplains are doing such a wonderful job dying to self, that they would stand there providing pastoral care,” said Carver. “The test of a true pastor is that they have words to sustain weary souls, that they really are a balm in Gilead. That’s what our chaplains are doing.”
Tele-chaplaincy
Phone visits and video-conferencing are becoming the norm, especially in the hardest-hit areas. In some cases, this is simply to reduce the risk of spreading the disease. In others, hospitals can no longer spare the protective gear to allow chaplains to visit in person.
In England, National Health Service went as far as saying patients dying from the virus should be encouraged to offer their farewells via video calls like Skype.
Veterans Affairs institutions have been conducting forms of tele-chaplaincy long before the current outbreak. Some institutions are also providing chaplaincy hotlines for patients to call, in addition to making resources available online.
“It is a different feel, for sure, because when I’m in the presence of a patient, and especially when I’m praying for them, I will typically hold their hand or place my hand on their shoulder, and then you’d have eye contact,” said Kinnersley. “On the phone, none of that is possible.”
Before coronavirus, he said he had only worked with one or two patients in his career that necessitated phone calls instead of in-person visits.
Some chaplains are getting more involved with broader spiritual care beyond one-on-one counseling with patients.
“A noticeable change for me is the focus on providing more support to hospital staff, being available to listen and help staff process anxious feelings and to help them reduce stress,” said Chris Mason, chaplaincy program coordinator for Augusta Health in Virginia. “If there is a surge, chaplains may be spending more significant amounts of time ministering to hospital staff, providing support to help them so they may continue to function at a high level.”
Chaplains are also sending “words of the day” via text and email, offering devotionals, and making use of social media.
“Every morning, I pray over the hospital loud speaker. Starting today, I’m sharing my #pandemicprayers. Pray for our hospitals and healthcare workers: nurses, docs, CNAs, security, dietary, EVS—all of us. And #GetMePPE,” tweeted Aimee Niles, a hospital chaplain in Portland, Oregon.
“#GetMePPE so I and other #chaplains can be present amid pain. It may seem like we aren’t essential, but we are. We’re what’s left when everything else has failed. And we are called to be there by our Creator. Let us,” she posted.
‘Light in Dark Times’
Complications around the pandemic don’t end in the ICU; they also stretch to funeral homes and cemeteries.
In Washington State, funerals have been massively restricted for a 15-day period. Georgia is seeing stricter guidelines as well, after infections were linked to a pair of recent funerals in the state. While CDC guidance currently states that funerals can continue, even for victims of COVID-19, some hospice chaplains have been restricted from leading funerals at all.
“I am hearing funeral homes, chaplains, and other clergy working together to find alternatives to large gatherings by using technology to bring grieving families and friends together and providing a means of honoring the memory of their loved one,” said Mason. “We recognize funerals, memorial services, and other similar types of observances are an important part of the grieving process and I am glad to see these continue, even though they are being conducted differently.”
Greider said one of the chaplains at her institution participated in a funeral service last week, conducting a simple graveside service rather than gathering in a sanctuary. An indoor service will be scheduled for a future date.
With COVID-19 infections continuing to rise—the United States had about 54,000 cases as of Wednesday—chaplains’ care has become even more essential, as other points of intimate contact for patients have been blocked.
“It’s important for people to be aware that spirituality does play a major role in the outcomes of patients, and the chaplain’s presence is important for more than just end-of-life care,” Bond said. “They are ambassadors of hope. They are guides who bring light in dark times. They are often seen as people who have been down this trail with others and can provide a comforting presence.”