Waving goodbye, I watch the glass doors close. On the other side, my mother stands red-faced, tears streaming, in the lobby of her assisted living community. Our family has a habit of damming up grief, but this is a pain neither of us can contain. I am crying too.
I leave my mother like this on the day I am tasked with delivering difficult news. On the advice of her physician and care team, my mother—officially diagnosed with Alzheimer’s two and a half years earlier—will be moving to the memory care floor. The move means admitting that she can no longer safely live without assistance. It means her Alzheimer’s is taking her into the deep end.
Everyone agrees this is the right choice, but that doesn’t ease my conscience. Am I acting prematurely to agree to the life-altering arrangement? Even after some desperate internet searches, it’s clear there is no objective measure of my mother’s readiness for the next level of care. The fog of my indecision mimics her own descending darkness, and I pray for a sign. It isn’t granted.
Thinking back now, the emotional truth of my mother’s disease had been plain long before her formal diagnosis. As many clinicians believe, dementia can creep in stealthily through the decades, diminishing function and often transforming personality.
After my husband, kids, and I moved to Canada in 2011, leaving my mother and stepfather in the US, the first signs of dementia showed up as passive, long-distance neglect.
Given the complications of cross-border shopping and shipping, my mother began to beg off buying Christmas and birthday presents for my children. So I dutifully ordered gifts on her behalf. When she complained about the geographical distance between us, I proposed, then arranged, her travel plans to visit us in Toronto. Every Sunday afternoon when I called, she sounded surprised, saying, “It’s been a long time!” The log of my resentments grew long in those years.
Then, in the summer of 2021, we visited my parents at their senior living community in Columbus, Ohio. It was our first time seeing them after 18 months of pandemic separation.
Dementia, as a clinical diagnosis, is largely a disease of deficit—impairments of memory, orientation, judgment, and executive functioning. During that weeklong visit, those deficits made their pathological presence known through excess, taking on a discomfiting pitch. The kitchen table was buried under months of unsorted mail and unpaid bills. The cabinets housed illogical quantities of hoarded items. In the refrigerator, Styrofoam containers of half-eaten food from the community dining room formed a blockade of spoilage and stench.
Was the clutter a symptom of my mother’s caregiving fatigue, given my stepfather’s deteriorating health? Or did it suggest something more sinister?
When I ventured to tell a neighbor that we were growing concerned for her, the woman—a longtime acquaintance from church—looked at me with knowing pity. “I think there are many who share your worries about your mother,” she said. I polled others discreetly, hoping for dissent, but that sentiment was only repeated.
Then, less than a year later, my step-father died—the same week we closed on a house in Cincinnati. I took control of all my mother’s practical affairs, and we left our life of 11 years in Canada to repatriate to America, moving my mother into a new senior living community eight minutes from our house.
Each time we invited her over for weekly dinner, she took to repeating, “I can’t believe we’re so close!”
At first, I corrected her. I wanted a little credit—and felt she owed me more than a little thanks. In truth, I was angry.
If I’m being honest, I do not know whose story this is. My mother and I are not the separate selves we imagine ourselves to be. Our stories were tangled from the womb, where boundaries between mother and baby are difficult to establish. In that secret place where God knit my inward parts, I drew life and breath from my mother’s body, and her health was my health. Is it still?
Over the past two and a half years, I have turned to science to puzzle together what’s happening to my mother. I am anxious to know, because dementia could quite possibly happen to me as my mother’s genetic heir. I want rational reassurances that I will not succumb to her disease. But I have yet to find any.
A 2025 Nature Medicine study states that US adults over age 55 have a 42 percent lifetime risk of developing dementia. One researcher told The New York Times that 6 million Americans are currently diagnosed with dementia. In 2060, that’s predicted to be 12 million.
I learn that, for all the technological advances we have made in medicine, we have made little progress in slowing the progress of dementia and other neurodegenerative diseases.
Although we’ve identified the genetic markers and observed (postmortem) the amyloid brain plaques and tau tangles often characteristic of Alzheimer’s patients, we also know that neither is a sure predictor of the disease. The widely accepted amyloid hypothesis, for example, has been more recently questioned by science reporter Charles Piller in his book Doctored: Fraud, Arrogance, and Tragedy in the Quest to Cure Alzheimer’s. Piller reports improperly enhanced photos of brain tissue appearing at least 80,000 times in scientific literature. That’s to say that, for decades, we might have been building a research house of cards.
I grow anxious about my own forgetting, certain on the worst days that any gap in my memory portends doom. I take up piano; I exercise religiously; I listen to the news in French. All of it is an effort to ward off the deterioration of my brain’s higher cortical functioning, the rationality without which it is hard to imagine existence. After all, I tell myself, studies show how healthy habits can improve cognitive functioning for at-risk populations.
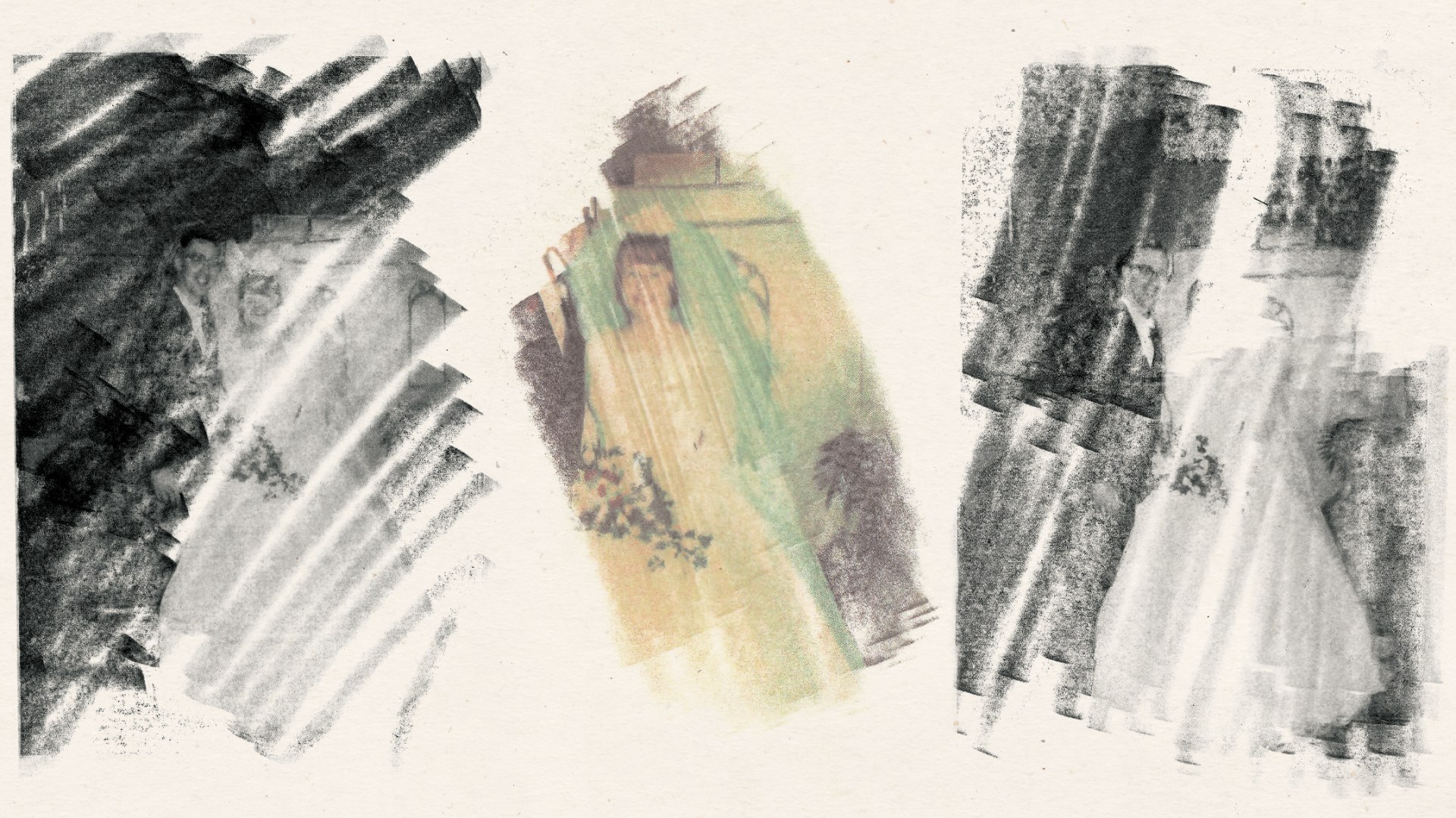
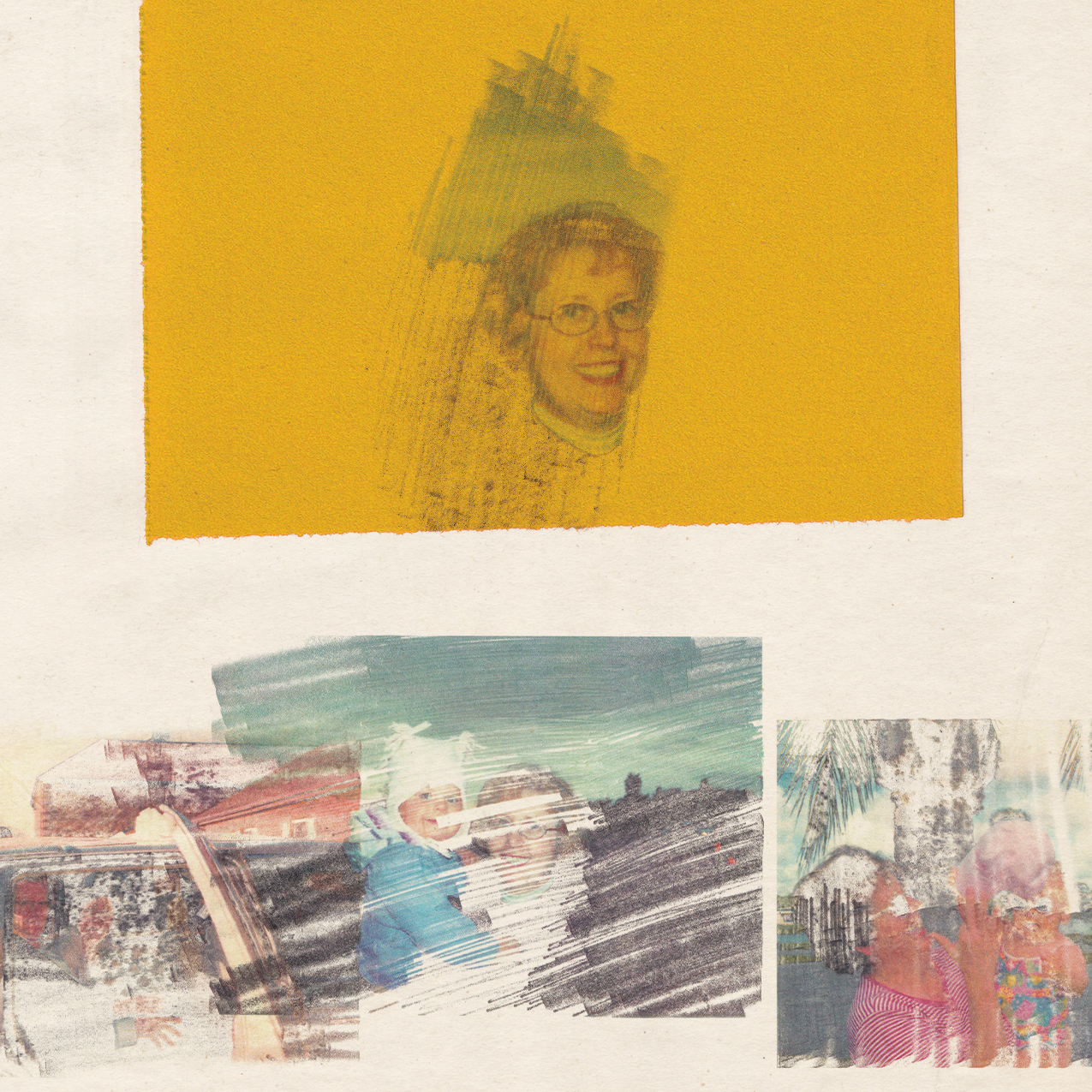
 Illustration by Vanessa Saba / Source Images: Courtesy of Jen Pollock Michel
Illustration by Vanessa Saba / Source Images: Courtesy of Jen Pollock MichelI wonder if my mother also tried to keep her faltering memory at bay. As a trained nurse, she once read popular medical literature touting the health benefits of blueberries, red wine, and daily movement. But if she had early anxieties about her cognitive decline, she never confided them to me.
Surely Alzheimer’s is the crooked line in Ecclesiastes 1:15 that can’t be made straight. There will be no healing for my mother this side of the veil. The darkness of dementia descends, and we cannot penetrate it.
“Do I have Alzheimer’s?” my mother asked me three times in the first year after her diagnosis.
Always, I told her the truth: Yes. I offered my answer plainly, as a dignity, even if the truth was terribly grim. She’d cry, and I’d put my arm around her shoulders.
But sometimes I fudge the truth now. I tell myself it’s for her sake. Like when she asks me, “Who is this man?” pointing to the loose photo lying on her table. Again.
“That’s my brother, David.”
“Is he still alive?”
I shake my head. His suicide at the age of 25 is now mercifully forgotten.
“How did he die?” she asks.
“In a car,” I reply, a partial truth.
“Oh,” she says with concern, though not grief. “He was too young to die.”
As my mother’s ability to tell her own story diminishes, I am becoming the keeper of her memories, for better or for worse. And as I tell her story—to you and to others—I realize I might also be telling my own. If I now beg God for mercy on her behalf, am I not, at least in part, pleading for myself?
Of the four apocalyptic horsemen of disease—diabetes, heart disease, cancer, and neurodegenerative conditions—dementia is the most feared, says Peter Attia, author of Outlive: The Science and Art of Longevity. Dementia is spoken of as a robbery of the mind, a theft of the self. Attia admits that his patients “would rather die from cancer or heart disease than lose their mind, their very selves.”
I watch as my mother’s days grow increasingly confined; she spends more and more time in bed. I would be lying if I said it was easy to believe what theologian John Swinton asserts: “Lives that are touched by profound forms of dementia have meaning and continuing purpose.” It seems blindly idealistic in the face of something so devastating.
What good can God intend for these days that travel the short distances from bedroom to bathroom to dining room to activity room? What good can God intend for my mother to forget her two previous husbands, her son, her grandchildren, and occasionally even me?
The story of forgetfulness is written in the unraveling of my mother’s once-capable life, but for her part, she expresses very little fear over the loose threads. After our routine lunch at my house after church, I dial her oldest friend and hand her the phone.
“Well, hey, Sis!” my mother says.
She is having a good day, and the conversation lasts longer than normal. At one point, I even overhear her thank the Lord for her good health.
On the October day we tell my mother she is moving to the memory care unit, her caregiving team and I sell the change with clever half-truths. There are so many more activities! There are wonderful new people you’ll get to know! We describe the “concierge” services that will soon be available to her: laundry, housekeeping, weekly manicures.
My mother is, at first, nonplussed. Our efforts at spin are, I think, largely successful—until the two of us are back in her apartment later that afternoon, and the stark truth of it all crashes in.
“What’s wrong?” I ask when she turns toward me sadly, an empty hanger in her hand.
“It’s just so much change all at once,” she says. “Why does everything have to keep changing?”
When I remember that moment now, it strikes me how much I hear echoes of Jesus’ words to Peter, foretelling the kind of death the disciple would face:
Very truly I tell you, when you were younger you dressed yourself and went where you wanted; but when you are old you will stretch out your hands, and someone else will dress you and lead you where you do not want to go. (John 21:18)
As the glass doors close between us when I leave later that day, I’m comforted that, at the very least, hers is a kind of end that Jesus himself knows.
The losses of dementia strike at the very capacities we are tempted to consider most deeply human: our language, our thinking, our memory. But rather than seeing it as a totalizing story of loss, the gospel invites us to consider the goods that flourish in the context of human weakness.
As much as we wish it were not so, we cannot straighten the crooked lines of human disease. Some sufferings are inexplicable this side of the eschaton. But we can remember that God is present with us, working out good, even in our most profound experiences of suffering.
I see God at work as my mother and I are engaged in a holy, human task: she in the dying, I in the giving of care that makes her dying easier.
Dementia, at the very least, reminds us of what it means to be human. We are fragile, finite creatures. We cannot self-exist or self-sustain. We depend on God for our very lives, but we are also deeply dependent on each other to offer the companionship and care that helps us both live and die.
Those losing their memories are teaching us about our mutual need, and those like my mother, who have cultivated a lifetime of deep faith in Jesus, are quietly inviting us into the way of the saint.
Amid the crumbling ruins of my mother’s mind, grace still finds her in the forgotten places. Some truths are rooted so deeply that even dementia fails to yank them up. Each time an old hymn is sung at church, for instance, she joins the chorus for at least a few bars. Even if her song of hope is weakened in the land of forgetfulness, God still hears.
Recently, when we pick my mother up for church, as we do each Sunday, I see a tender bruise of blue above her eye. My first thought is that she fell—one symptom of dementia. When I reach out my hand to touch the bruise, though, it smears: eyeshadow.
She doesn’t remember putting it there. As I wipe her face, she gives herself peaceably into my hands. That submission is a gift I don’t take for granted. I receive it, and I pray for gentler hands. Having practiced presence with her these last two years, I am thankful I can now receive my mother as she is, honoring the best memories of who she once was.
These days, when I stoop to zip my mother’s coat, I go all the way down and kneel, the way she must have once done for me when I was little. I’ve come to assume it as a posture of prayer, saying the words of a liturgy from Every Moment Holy, Volume II:
Let me love well this one who suffers. Let me again and again choose love in each moment, so that through every small act of care and mercy the practice of love becomes a liturgy and a habit by which you are forming in me a compassion that cannot be learned any other way, save by the giving of myself in long service to another.
As I pray, I craft a new vision of my mother, myself, and the story we’re living together.
Genes are not the only thing my mother has given me. I remember how every morning, as a child, I would shuffle down to the kitchen and find her head bent over her Bible in prayer. She faithfully prayed for me on the days I didn’t know how—a generational gift of surpassing worth—and now I pray for her.
Even though she may have forgotten those mornings, and someday I may too, God will not. And when she and I awake someday into the new world, God will wipe away each tear as we remember.
This is the story we are both living: tragic, but not left unredeemed or unrecorded. From the very beginning, before we drew our first breath, in God’s book were written the days that were formed for us, every one of them. Our story is, in the end, his.
How precious are the thoughts of God; how vast the sum of his remembering. Today, it is enough for me to know this, both for myself and for my mother.
Jen Pollock Michel is a writer and speaker. Her books include In Good Time: 8 Habits for Reimagining Productivity, Resisting Hurry, and Practicing Peace.