“It would be better to die than to suffer this way,” Fathia says, wiping her hands together with finality. She sits across from me at the Caritas medical center in Djibouti, crying. I’m trying not to cry. I’m also trying not to back away as she coughs without covering her mouth. She is a single mother, a refugee from Somalia, and all five of her children have tuberculosis, commonly called TB.
According to the World Health Organization, close to 50 people are infected every week in Djibouti—a massive percentage for a small country with a population of less than 1 million. The disease is transmittable by air, a fact that I’m well aware of while we talk. A person of my healthy constitution and plentiful diet is unlikely to develop an active case of tuberculosis. And yet I know American lawyers who have had active TB. Diplomats. Teachers. Students. People just like me. The disease is in New York City, in Minneapolis, in Paris.
Like other infectious diseases that plague the modern world, the cure to TB is complicated. But because of the social stigma and isolation associated with it, medical professionals are increasingly convinced that part of the solution will come from one simple source: trust born of relationships.
“A trusting relationship is critical,” says Annie Mikobi, a Congolese doctor working in Djibouti. “Without it, there is no observance of treatment.”
“Stigma is a huge barrier, and breaking down stigma requires trust,” says Bob Carter, a family practice doctor with SIM (Serving in Mission) who has worked with TB patients in Kenya and Zambia for over 20 years. “TB patients must trust that I care about them, that I won’t disclose their status to others, and that I have their best interests at heart. When healthcare providers are not trustworthy, those living with infection remain hidden.”
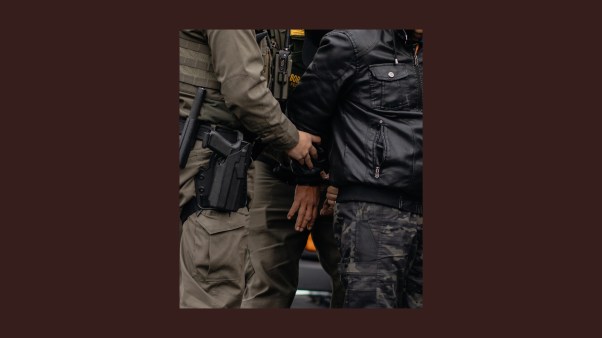
Here in Djibouti, a person with tuberculosis might be kicked out of their home. Family members might refuse to eat with them or to sit in a room with them, and they aren’t welcome at community events or even offices and schools. In other words, Fathia and her children are modern-day lepers.
“It’s like we’re dead already, anyway,” Fathia says. “Kids won’t play with my children. They run away from them in the street. People talk about me. They say, ‘Look at that mother. She made all of her children sick. She is a terrible mother.’”
Although the doctor at Djibouti’s Hol-Hol refugee camp provides free tuberculosis medications, Fathia left the camp and came to the city in order to earn money by begging. She brought only the pills she had at the time, enough for seven days.
Now Fathia gets pills at a center in town but is inconsistent in how she administers them. Sometimes she gives the youngest one all the medicine and sometimes she spread the pills out among the others. No one regulates their care—what doctors call “directly observed therapy”— and they are all getting sicker. They cough through the nights and huddle together under blankets trying to keep warm while their lungs devour themselves. Her youngest, Yusuf, faints on a daily basis.
“I have fevers. I’m coughing a lot,” she says. “But I can’t go to the doctor. I can’t leave Yusuf or he will fall into a fire, fall on the stones.” She coughs again, this time into the blue and red cloth of her headscarf.
Until now, Fathia hasn’t understood that by administering the pills so inconsistently, she is possibly giving them multi-drug resistant TB—a death sentence for a refugee in Djibouti. At the very least, she isn’t curing them, and they could be infecting neighbors or friends. Although it might be easy to judge Fathia for failing to follow the doctor’s recommendations, her refugee circumstances bring a unique level of desperation and chaos.
“Successfully implementing DOTS [directly observed therapies] in a public health TB program in stable communities is challenging enough,” says Carter. “The difficulties are multiplied many fold in migrant or refugee populations.”
With Fathia in front of me, I am reminded of the lepers of Jesus’ day who suffered from the same fear, loneliness, and social marginalization. Jesus touched their disease and in doing so, he restored not just their health but also their place in the community and their sense of dignity. He made them clean and whole.
While I don’t have the healing power of Jesus, I do hope to hear and affirm Fathia’s story without being afraid of what floats between us, without shrinking back. The call of the gospel is to go to the jails and slums and medical clinics and to offer dignity, affection, and humanity. In other words—to establish relationships like this one that build trust and extend Christian love.
Medical professionals, in particular, know the faith community is key to the TB cure. “Our response to tuberculosis and AIDS would not have been and will not be the same as it is today without the faith community, and now there are five critical actions we need to take together,” Eric Goosby, United Nations Secretary-General’s Special Envoy on Tuberculosis, said at a UN interfaith prayer breakfast last September. “Educate, advocate, and fight stigma. Continue to fight for patient-centered care. Give voice to the voiceless, especially the children.”
I’m not a medical professional and I have no control over cures, but I can direct Fathia to the pulmonary care nurses at the social service center where we sit. We can talk about inexpensive, healthy meals for her family. I can urge her to be consistent with the pills and to allow a medical caregiver to supervise her family.
As Fathia coughs, I think about Jesus touching lepers and place my hand on her shoulder. I pray she will trust me enough to take my advice. That’s the closest I can get to a miracle.
Rachel Pieh Jones is the author of Stronger than Death: How Annalena Tonelli Defied Terror and Tuberculosis in the Horn of Africa, slated for publication in October 2019. Get all her stories and updates in the Stories from the Horn newsletter.