Medical professionals across the US are preparing COVID-19 units in a suspenseful quiet, while others in places like New York are already overwhelmed with patients. The city has ordered hospitals to increase capacity by 50 percent, and they are looking at ways to use temporary facilities, including a recently arrived Navy hospital ship, hastily built field hospitals, and even hotels.
In the midst of all this, doctors and nurses are preparing to face agonizing ethical decisions as their Italian counterparts have already in recent weeks. According to some estimates, the number of projected coronavirus patients needing ventilation in the US could reach anywhere between 1.4 and 31 patients per available ventilator.
There are three main ethical concerns that medical professionals are now facing, according to the Center for Bioethics and Human Dignity: protecting the vulnerable by not overwhelming health care systems, allocating insufficient medical supplies, and keeping medical workers safe who lack the proper protective equipment against the virus. The questions are very real: Who should receive medical care when there aren’t enough resources to go around?
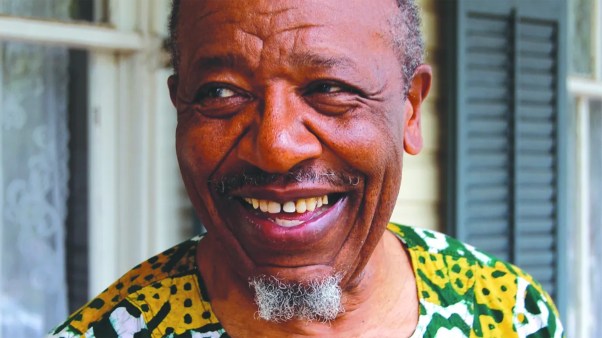
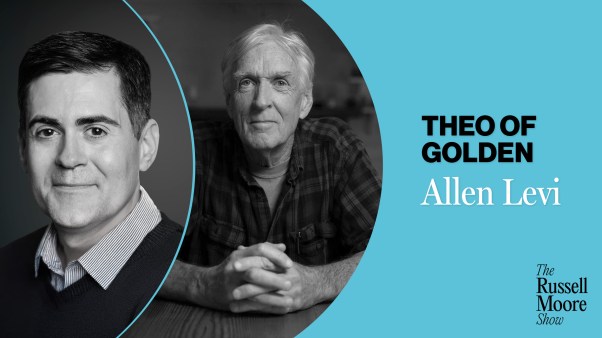
Two ethicists aiding US medical workers with these dilemmas are Carol L. Powers, a lawyer and the co-founder and chair of the Community Ethics Committee out of Harvard Medical School’s Center for Bioethics in Boston; and David Stevens, a physician and CEO emeritus of the Christian Medical & Dental Associations in Bristol, Tennessee who spent 11 years on the front lines of the HIV/AIDS and malaria epidemics in Africa.
CT spoke to Powers and Stevens about how Christians should approach issues of life or death.
How does the relationship between the physician and patient change during a public health crisis like a pandemic?
Powers: In the normal course, the physician-patient relationship is shaped by two different “spheres of decision-making.” Typically, the patient is charged with articulating their individual goals of care based upon their personal values and preferences. The physician then responds with various treatment options that would accomplish those individual goals of care.
In a public health crisis where health-care resources become limited, the physician-patient relationship changes drastically. The weight accorded to an individual patient’s goals of care diminishes in light of the community’s increased need for health care resources. Rather than focusing solely on the patient in the bed, the physician must now consider the many patients in many beds. Treatment options available to both the physician and the patient become necessarily limited.
Critical care resources—an isolation unit or an ICU bed or a ventilator or dialysis—may not be a treatment option offered or it may even be withdrawn. In the case of non-critical medical needs, surgeries or treatments may be delayed or become completely unavailable. Resource allocation questions force a shift in the physician-patient relationship so that the patient’s desires for specialized medical treatments cannot be accommodated and the physician reluctantly becomes a gatekeeper for access to any care at all. Medical care that was once assumed to be available may become limited or completely unavailable.
For the physician, an uncomfortable shift occurs from providing patient care supported by evidence-based medical standards offering a full panoply of treatment choices to operating under crisis standards of care providing limited treatment options in an attempt to save as many people in jeopardy as possible.
Whenever the question arises “what should we do?” then you are in the arena of ethics. The focus of decision-making in ethics often centers upon balancing benefits and burdens of competing “good or right answers.” In our pre-March 2020 world, a patient was able to exercise a good deal of decision-making authority about what treatment options they wanted based upon an ethical decision-making principle of autonomy. In our post-March 2020 world, the ethical principle of justice asserts itself and physicians must find ways to allocate limited resources in ways that are fair and do the most people the most good. For years, we have stayed away from talking about rationing health care and now, because of a crisis beyond our control, we are being forced to ask hard resource allocation questions.
How are medical professionals making decisions about who to prioritize for care?
Stevens: The four basic principles of ethics [include] beneficence, which is doing good; non-malfeasance, which is doing no harm, justice, [and autonomy], and all those things are impacted by an epidemic.
You have the ethical quandary of, do I take care of the sickest folks or do I take care of the most folks? You focus on those in the middle. You have those that aren’t very sick, you tell them to stay home. And then you have people who are desperately sick and when there are not enough respirators, there’s going to be a decision-making situation where you’re going to say, this person is so sick, I’m just going to sedate them or give them something for pain or air hunger, but I don’t have the resources nor the time to focus on this person to the detriment of 15 others who are moderately sick who I can save. That is what we call competing goods. Both of those are good things but you can’t do both.
I remember as a young missionary in Kenya, we had a lot of premature births—some of the highest in the world because we had the highest multiple births—that one out of every 28 deliveries was a set of twins. So we had a lot of preemies. We didn’t have 24-hour electricity. We had a little generator we could use to run one isolette. You can put three premies in an isolette, but what do you do when the fourth one comes? I had to make this decision many times and say, Okay, great, this one’s doing better. I think we can take it out and put this one in. But other times you looked, and all of them were doing bad and you think, this one is so bad in the middle, I’m going to take that one out and just give it comfort care and give it back to its mother and I’m going to take this other one that was just born and is doing better and put it in.
Well, that’s not fair. You can’t be fair in these types of resource-depleted situations. And you get into what we call utilitarian ethics of doing the best you can to save the most people when you can’t save them all. You do that while not violating any moral absolutes.
Powers: There are several different ways to allocate scarce medical resources. One could argue for a first-come, first-served system or even a lottery. What most hospitals are instituting are crisis standards of care that are that trying to maximize the most life years. What that means on a practical basis is a patient with COVID-19 whose health is already compromised by other life-threatening medical conditions may not receive as much intensive medical support as someone whose health is not medically compromised.
Doctors are trying to assess who will benefit the most for the longest when they offer access to scarce medical resources. It means hard choices are inevitable, especially because we have come to rely on the physician acting as an advocate for their individual patients. In order to keep that relationship intact as far as possible, hospitals are now putting into place triage teams—clinicians who are not directly providing care to a patient—who evaluate the test results and determine who will be most likely to benefit the most.
Stevens: One of the premises of medicine is you do no harm. We are taught in health care in this country that you never do anything you’re not trained to do, that you’re not competent to do. We’re already moving past that in New York because you’re going to have people that haven’t practiced medicine in years coming back to help out. This is a place where you have to do that. There’s a place when you’ve got a moral duty to help people, but you have a conflict. And you’ve got to set priorities and you have to allocate limited resources. All these things play into it and make it a very difficult situation, especially here in the US where people haven’t had to deal with these things.
How are these policies formed? Who is involved in making decisions?
Powers: Because these policies are being formulated under duress in exigent circumstances, the opportunity for community review is limited. Harvard Medical School’s Center for Bioethics has provided some resources to a Community Ethics Committee which I have overseen for the last 13 years. It is a diverse group of community members that provides review and comment on hospital policies. We were asked to comment upon a draft policy promulgated by some of the hospitals within the Harvard system and we are working on drafting informational materials to help the public navigate these turbulent health-care waters. A sister group at Yale called the Community Ethics Forum has also been looking at this topic.
Stevens: At a hospital level, there are ethics committees, there are administrators, there are chief of staff, physicians, and others. But often ethics committees have the time to do this. The trouble in these types of epidemics is that you don’t have that time as things get worse. You have to essentially trust your doctor. It gets as basic as that.
Powers: Even if we were able to provide robust community input, the problem lies in the fact that incredibly difficult medical decisions will have to be made at the bedside with limited time and limited knowledge of the patient’s life and values. The volume of patients needing intensive care could potentially require a total reliance upon a team of clinicians deciding access to critical care resources based on the results of medical tests and nothing more.
Each community member can be involved in their own health care by educating themselves about advance care directives. Health care proxies should be signed and personal values that inform choices for medical care should be discussed with family members. Proactively, each one of us should reach out and mend broken ties to the extent we can. We need to tell our loved ones how important they are to us. And goodbyes should be said now. That sounds like a drastic recommendation but given the prohibition of hospital visitors, we need to do now what we may not be able to do later.
Do people have a right to palliative care in the event that there is not enough equipment? If that isn’t possible, how are medical professionals thinking through dignity at the end of life?
Powers: The dignity each of us experiences at the end of life is provided not by who is at our bedside or what medical treatments have been made available to us. The dignity each life has is based upon the image of God bestowed upon each of us—with our first breath given to us at our births to the last breath taken at our deaths, our dignity is based upon our relationships with each other and our God. Because our God will never leave us or forsake us, he will be with each one of us as we die. It is our loved ones who will need that sense of dignity—a sacramental leave-taking —that may be missing in this world of isolated dying. To my point above, we all should spend this time in closing accounts—communicating our love and showing our respect and giving our blessing —with those we love. Therein lies our dignity.
Stevens: You always want to provide comfort even when you cannot provide a cure. That’s not difficult. It doesn’t mean people have to physically suffer, as long as the medications last. You always want to show compassion as best you can.
How should Christians think about these ethical dilemmas?
Stevens: For Christians in health care in particular, you’ve really got to dig into God’s Word. One of the verses that really helped me as I dealt with these things for 11 years [in Africa] was 2 Timothy 1:7: “For God had not given us a spirit of fear, but of power and love and a sound mind.”
It means you pray for wisdom and help [patients] with compassion. People care less that their doctor can cure than that they really care. If they know they care, they know they’re doing the best that they can.
For centuries, Christians have not run away in situations like this in a crisis—they’ve run to them. I think this is a tremendous opportunity for Christian health-care professionals—and of course, I deal with 35,000 of them—it’s a great opportunity to demonstrate Christ, not just in word, but in deed. That’s the good news—that we don’t have to fear. God is still in control. I didn’t walk home in the middle of an epidemic [in Africa] afraid to death for my wife or kids. I took reasonable precautions and then trusted God. I realized he was in control. He called me there and this wasn’t a job. This was a calling.
Kara Bettis is an associate features editor at Christianity Today.