In Malawi, medical records look a bit like passports: little blue books emblazoned with scribbles and ink stamps. When Agnes Moses was starting out as a doctor at a Christian hospital there more than 20 years ago, one stamp would bring her spirits low.
In those days, no treatment was available for patients diagnosed with HIV. So doctors would write an order in patients’ books for spiritual counseling. After a visit, the counselor would stamp the page by the doctor’s notes.
“To me that was a death sentence, every time I saw the stamp,” Moses said. At the time, about a third of the patients in her ward had HIV. She lost medical colleagues and members of her church to the virus, too. In southern Africa especially, hospitals were overwhelmed with dying patients.
A United Nations report in 2000 was grim, predicting that as many as half of teenagers in southern Africa would die early due to AIDS. In 1998, 30 percent of pregnant women in Blantyre, Malawi, were testing positive for HIV. Life expectancy in Malawi that year was 43 years. In sub-Saharan Africa, the epidemic was hitting women much harder than men.
In Botswana and South Africa, life expectancy dove by about a decade as HIV took over in the 1990s. “We are threatened with extinction,” Botswana president Festus Mogae said in 2002, when 39 percent of adults in his country were infected with HIV.
There was a way to make HIV a survivable condition: Effective antiretroviral therapy (ART) had been developed in 1996, but few had access to it.
In 2003, president George W. Bush convinced Congress to pass the President’s Emergency Plan for AIDS Relief, or PEPFAR. It was an unprecedented global health program, appropriating about $5 billion a year to fight AIDS. With a laser focus on clinical treatment, PEPFAR distributed money to many existing African programs and clinics. It created a separate infrastructure out from under other federal agencies and stricter-than-normal reporting requirements on distribution of funds. The number of people on ART in Africa scaled up from 50,000 in 2003 to 20 million in 2022.
Instead of facing extinction, Africans have seen their life expectancy shoot up by 10 years since 2000—a greater increase than any other region in the world experienced over the same period. Today, 91 percent of adults and children with HIV in Malawi are on treatment. (Most ART funding in Malawi comes from the Global Fund, a multinational program largely financed by the United States, as well as from PEPFAR, which is entirely US-funded). Prevention campaigns are working, too: From 2010 to 2021, new HIV infections in Malawi decreased by 61 percent.
“It was the closest I’ve ever come to seeing the miracles of the New Testament … to see people near death come back to life,” said Bush speechwriter and PEPFAR advocate Michael Gerson in a 2019 video.
The US government estimates that PEPFAR has saved 25 million lives. The program currently supports 20.1 million people on treatment—mostly in Africa, but also in places like the Dominican Republic, Haiti, Ukraine, and Vietnam. Most Americans don’t know the program exists. Bush joked at an event last year that when a Texan hears about PEPFAR, they’ll ask, “Is that a toothpaste?”
But the little-recognized program is evidence that people of widely differing viewpoints—African leaders, LGBT activists, American evangelicals, Republicans, Democrats—can do something big together and do it well, something that saves lives and that endures. “It is in our human nature to better respond to emergencies than to sustain efforts over time,” said an Institute of Medicine report evaluating PEPFAR in 2007. “The energy, empathy, perseverance, and technical competence of those implementing PEPFAR will be needed for many years into the future.”
Somehow, PEPFAR has been repeatedly reauthorized by Congress for over two decades. But funding for the millions who depend on ART treatment is a question mark every year. Absent some new scientific breakthrough, HIV patients have to remain on those drugs for the rest of their lives. The program is fragile because people do not remember what a big thing many nations did, and are doing, together.
“We worry all the time” about funding stopping, Agnes Moses said. “By the grace of God, we have been able to survive and be a little bit sustainable.”
The worry is not unwarranted. Funding for PEPFAR decreased slightly under president Barack Obama, even as the program’s advocates were pushing to scale it up. President Donald Trump repeatedly attempted to slash the program by more than 20 percent, including eliminating funding to seven countries entirely. Congress rejected those proposals, but legislators have put up their own obstacles over the years—such as when, in 2008, Senate Republicans placed a three-month hold on PEPFAR’s reauthorization, accusing the program of “irresponsible spending.”
This year, Congress will need to reauthorize PEPFAR as a program for another five years (a separate process from annual appropriations). Reauthorization always revives tussles about PEPFAR’s place among federal agencies and how much independence it has. Bush structured the leadership to have a direct line to the president as a way to ensure the program remained a priority.
Will the United States continue to support the millions of people it has put on lifesaving treatment? And was the success of PEPFAR a one-time stroke of grace, or could a sustained bipartisan project like it happen again?
Africans who had seen many foreign aid programs come and go initially met the program with skepticism. “I didn’t know how this was going to change things on the ground,” Moses said. Even if the US money came through, Moses knew in Malawi she would have to contend with the stigma of submitting to testing for HIV as well as Malawian beliefs in traditional remedies over pharmaceutical drugs.
Policy wonks, international aid workers, and HIV doctors shared Moses’ skepticism that PEPFAR could work.
“This was not a foregone conclusion,” recalled Mark Dybul, one of the architects of the program who later became the head of PEPFAR under Bush. “Everyone who looks back on it now is like, ‘Oh, of course, PEPFAR.’ … It could have fallen off the rails a thousand times, especially in the early years, for implementation and political reasons.”
In the United States in the 1980s and 1990s, Christian compassion toward HIV/AIDS victims emerged, in some cases, from grief like what Moses felt in Malawi. Gerson’s close friend and suitemate at Wheaton College died from AIDS a few years after they graduated in 1986. The death “was devastating to him,” Gerson’s brother, Chris, remembered. “At a very early age, he put a face to that epidemic.” Gerson became Bush’s speechwriter and was a key advocate in the administration for a global AIDS program, along with then–national security advisor Condoleezza Rice. (Gerson died in 2022 from cancer.)
In the 1980s, American churches—like much of America—were still overcoming misinformation and stigma about AIDS.
In 1985, Baptist pastor Scott Allen learned his wife and children were infected with HIV that his wife had acquired in a blood transfusion. Upon learning the news, his church asked him to resign. His baby son, wife, and eventually his other son died from AIDS.
Around that same time, Shepherd and Anita Smith—evangelicals who felt prompted to be involved in HIV policy because of Shepherd Smith’s physician father—received a CDC grant to do outreach to churches about HIV/AIDS. So little was known about the virus that they spent most of their time debunking rumors.
At one event in Colorado in the late ’80s, Anita Smith remembered meeting a woman whose five-year-old son had HIV. With no treatment available and facing her son’s escalating illnesses, the woman asked for help to pay for rent and groceries. Anita Smith suggested asking a local church. The woman told her that the church had agreed to meet with her but asked her not to bring her son.
“It was just like a knife in the heart,” Smith said. She and her husband started an emergency assistance program—partly using their own money—to help people travel to see family members dying of AIDS or to pay for burials. They paid for rent, groceries, and car repairs. They did a holiday gift program for children who had HIV or were affected by HIV.
 Getty / The White House
Getty / The White HouseThose were lonely years to be evangelical AIDS activists. “There weren’t many people in the evangelical community who saw this as an issue that involved them,” Shepherd Smith said. “It involved things that the church wasn’t really capable of dealing with, like homosexuality, like drug abuse.”
Meanwhile, a more activist public-health contingent ridiculed the Smiths because of their support for abstinence education as a part of HIV prevention and because of their position that HIV-infected individuals should notify partners of their condition. Gay activists would come to their talks at churches and record them. Shepherd Smith said he and his wife were threatened once over an amicus brief they were planning to write on HIV prevention; they decided not to write the brief.
“Being gay was not an issue with us” when it came to public health, he said. “Where we differed was on values.” Some activists opposed pushing monogamy as part of the solution. But the Smiths believed that, to slow the spread of the virus, “faithfulness was an important element in adult relationships. Having one lifetime partner should be everyone’s goal—it didn’t matter to us whether it was gay or straight.”
As time passed, the Smiths set up a global AIDS nonprofit that supported local organizations in Africa doing AIDS care, and politically they were the early and essential evangelical advocates pushing for PEPFAR.
By 2003, the HIV virus was busy killing off a generation of Africans. Tensions were high about how—or even whether—to provide antiretroviral treatment globally. A Washington Post investigation in 2000 uncovered internal memos from USAID, the development arm of the State Department, in which one AIDS official said “overpopulation” was Africa’s biggest problem. Another memo argued that treatment in Africa would “siphon off resources” with “limited or no impact on the course of the epidemic.” A World Bank study noted that the reduction of Africa’s population through AIDS “would increase the growth rate of per capita income in any plausible economic model.”
Mark Dybul, who went on to run PEPFAR and later the Global Fund, remembered Bush being “infuriated” about the implication in public health circles that Africans couldn’t handle antiretroviral therapy. One USAID administrator had said Africans wouldn’t be able to adhere to the timing of the drugs because they didn’t use clocks. Dybul recalled a meeting at the World Bank two years into PEPFAR where someone said they should halt ART in Africa because, if patients didn’t follow the regimen, a drug-resistant HIV would hurt the US. (That didn’t happen.)
Bush was walking into all of this when he announced the massive HIV/AIDS program in his 2003 State of the Union address. A few top HIV experts, including Dybul, and White House aides had been meeting secretly to plot out PEPFAR. They didn’t want Washington’s entire bureaucracy to find out about the plan, for fear the proposal would be torn apart by competing interests. Dybul remembered Anthony Fauci, then an AIDS adviser to the White House and a legendary HIV researcher, calling him repeatedly on the day of the address to double check the language Gerson had written announcing the plan.
“The politics of it got very intense very quickly. Everyone hated it. The Left, the Right—everyone hated it,” Dybul remembered. There was “enormous resistance” to funding faith-based organizations in Africa. But they were a key part of the plan, because although PEPFAR did have a goal of building local governments’ capacity, faith-based health facilities and NGOs were the only viable medical providers in some places, especially rural areas. “They were the ones running hospices,” Dybul said. A conscience clause in the legislation—which included allowing Catholic providers receiving funds not to provide abortions or birth control—was key for getting faith-based health care providers to participate.
 Getty / Paul Morigi
Getty / Paul MorigiThe political battle made for strange alliances. Dybul, one of the key architects of the program, is gay. He admitted that, at the time, he hated Bush and thought he had stolen the 2000 presidential election. Dybul was skeptical about PEPFAR, thinking it would be merely symbolic or maybe worse. “[I] assumed everyone around [Bush] was evil and up to no good,” Dybul said in an oral history of the program. “Then I got to meet them. They really are some of the most remarkable—They’re still all good friends.”
Senator Jesse Helms, who along with his caustic remarks about homosexuality had also previously referred to development aid as going down “foreign ratholes,” came around to be a major supporter of PEPFAR after lobbying by senator Bill Frist, a doctor who had gone on mission trips to Africa; Bono; and Franklin Graham. Frist’s office arranged for Helms to meet an African woman with HIV and her baby, according to To End a Plague, a history of PEPFAR by AIDS activist Emily Bass. Helms began to cry and pledged his support.
The legislation passed in May 2003 after much wrangling over funding, abstinence (it was allowed as a prevention measure), and abortion (Bush exempted PEPFAR from the Mexico City Policy, a Reagan-era rule that barred groups that received certain types of US health funding from performing or encouraging abortions).
US leaders modeled the program after a local treatment strategy pioneered by a Ugandan doctor, Peter Mugyenyi. Dybul had spent time watching Mugyenyi’s work in Uganda and was amazed to see community health workers motorbike out to villages to do tests and provide drugs. People in villages knew their CD4 cell count, their viral loads, the names of the drugs, and when to take them. “The community health care workers were like these little angels,” Dybul said. Dybul got all of Mugyenyi’s data about costs, then used the numbers to build out goals for a bigger program. He engineered it around a “wheel-and-spoke” health delivery system similar to one used by the Indian Health Service in Alaska.
“One of President Bush’s unconditional aspects of PEPFAR was that it not be top-down. That we’d be supportive and servants, and that we’d be respectful and humble,” Dybul said. “It’s the only way for a sustainable, long-term approach.”
Within six months of PEPFAR’s launch in Uganda in 2004, the number of Ugandans on ART doubled. In Rwanda, after PEPFAR sites were operational for two months, hospitalizations fell by 21 percent, according to officials’ 2007 testimony in Congress.
Sustaining PEPFAR requires an interest from the American people in the lives of people who are thousands of miles away.
“Politicians need permission from constituents to do the right thing,” said Tom Walsh, who was a top PEPFAR official for years and is a Christian. Walsh underlined that funding PEPFAR every year is a battle. “It’s important for politicians to get that permission, to counterbalance the voices telling them, ‘We have problems at home, and our money needs to stay here.’ … In America, many Christians are influential. Their voices are listened to.”
Christians who were involved in HIV advocacy for decades think that if the church is going to be involved in something big like PEPFAR in the future, it needs leadership and education.
Saddleback Church’s Kay Warren was an early evangelical booster for HIV/AIDS treatment in the United States and abroad. She had been heartbroken by stories of Africans with HIV. But she said everything she thought she knew about HIV “was wrong … and full of stigma and judgment.” She received a detailed education about the virus from HIV doctors she got to know. “God got my attention,” she said.
In 2004, Warren was just coming back to ministry after breast cancer treatment when she asked the congregation if they would be willing to work on some kind of HIV response. She said she got 3,000 responses from people wanting to help. She and her husband, Rick, held HIV summits at Saddleback and staffed an HIV ministry for domestic and international care. At the summits, attendees met people who had HIV. “We humanized it,” Warren said.
The Warrens became key backers of PEPFAR alongside the Smiths, rallying evangelicals over the years to support the program and prodding politicians on Capitol Hill when the program’s budget came under repeated threats. After their son’s death by suicide in 2013, the Warrens shifted their personal focus to mental health and Saddleback’s AIDS program diminished—illustrating the importance of sustained leadership on an issue.
Walsh, who went from working for PEPFAR to working for the Bill & Melinda Gates Foundation, said PEPFAR helped the wider development world see what faith-based organizations could contribute. “The view of the faith sector in the development and health world is much more collaborative or welcoming now than it was almost 20 years ago,” he said. “It’s much more established that faith organizations have a lot to contribute.”
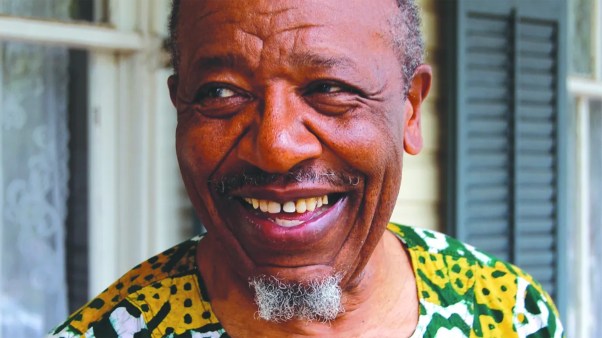
In Lilongwe, Moses now leads a major Christian medical center for HIV patients called Partners in Hope (PIH), which administers PEPFAR funds. An American missionary, together with Malawians, established the treatment facility in 2001—before PEPFAR. It was one of the earliest such facilities to scale up to a national level. PIH now administers a network of 123 facilities that together provide antiretroviral therapy for 20 percent of Malawians who are receiving treatment, according to Moses.
It’s not unusual for a faith-based health center to oversee so much HIV treatment. In Malawi, 70 percent of rural health care comes from church clinics and hospitals, and most of the population is rural. Faith is “in every thread of our treatment,” Moses said. PIH provides spiritual support for those with HIV—and “elimination of prejudice against HIV.”
 Maria Thundu for Christianity Today
Maria Thundu for Christianity TodayMalawi is one of the poorest countries in the world; physicians are overloaded, and brain drain is a problem. Moses could have left but didn’t: “I like to help people come out of their hopeless situations.” She came from a village; her father died when she was a child and her mother was illiterate. She and her siblings went to school and taught their mom how to read.
As a doctor, Moses contributed to pioneering research and treatment for HIV/AIDS patients in Malawi, especially in preventing mother-to-child transmission. Such Africa-based research is important: Moses’ work demonstrated, for example, that Malawians had better outcomes if they started antiretroviral therapy with a higher white blood cell count than doctors had previously recommended.
On a sunny afternoon at PIH last year, a waiting room television played a local gospel music video to rows of empty benches. Nurse Loveness Mang’ando, working that day, remembered 20 years earlier when the medical center was full of “very sick patients with HIV.” Now patients just come to refill their medications: “They are stable.”
The medical center exemplifies how HIV treatment helped build the nation’s health infrastructure. Because people are living longer, the clinic has turned its attention to treating diabetes, hypertension, and other noncommunicable diseases. In 2020, PIH launched a surgery department, and its lab is the envy of many less-resourced hospitals—with diagnostics on everything from liver function to tumor markers to HIV viral load. When the coronavirus broke out, the clinic turned some of its unused HIV beds into a COVID-19 ward. “We have space to think about other conditions now that HIV is under control,” Mang’ando said.
Malawi still has problems. So does PEPFAR more broadly. People with HIV still wait too long to come to PIH for help, which means they are more seriously ill when they arrive. And there are stubborn pockets of new HIV transmissions. But compared to two decades ago, “It is not the same world,” Moses said.
“It’s unbelievable,” she added. “It feels very satisfying that, as a country, we have moved. We cannot eliminate HIV, but at least it has been contained. At the same time, I feel sad. I wish this happened earlier—that we were not going to be seeing so many deaths.”
In 2003, when PEPFAR launched, Malawi’s average life expectancy was 49 years. Now it is 65. Moses, age 50, jokes that she is in her second life.
Emily Belz is a news writer for CT.