After 10 months of limited in-person gatherings or online programming, church congregants—like the rest of society—feel pandemic fatigue. We are hopeful that the availability of COVID-19 vaccines will allow our society and churches to return to normal. But a return to normalcy will take time.
Unfortunately, many of our Christian brothers and sisters living in low- and middle-income countries, where I have worked for more than 25 years to stop the spread of infectious diseases, will not receive vaccines until 2022 or later. In countries like the US where the rollout of COVID-19 vaccines began last December, experts predict it will be fall before vaccination coverage reaches 70–90 percent and herd immunity can hopefully be achieved. Only then can society begin to resume more normal activities. The next several months will be a transition period when vaccinated and unvaccinated individuals mingle in our communities, but it is not yet safe to return to normal life.
During this transition period in the US, how should church leaders decide on in-person gatherings for their churches? Because vaccination will proceed at different rates in different communities and vaccination of church congregants will vary even among churches within the same community, there is no single approach to regathering.
In consulting with four churches in my home city of Seattle to plan for this transition, I've seen leaders struggle with the complex issues before them. James Broughton, the senior pastor of a predominantly African American congregation said, “This is such a complicated situation—with so many moving parts. We really need godly wisdom, which includes scientific knowledge, to know what to do.” All those I talked with see the need for open discussions within the church and the value of having a plan before churches are confronted by different pressures to regather.
To navigate this transition period, I will explain how COVID-19 vaccination influences decisions about church gatherings and provide five suggestions that can help churches develop a plan to regather as vaccination coverage increases.
As in my previous CT articles on church gatherings during this pandemic, I have tried to discern God’s call for his church using two guideposts: biblical truths and scientific knowledge, both of which have been given by God.
How COVID-19 vaccination influences church gatherings
Explicitly stated or not, church leaders are balancing three factors when they consider church gathering during this pandemic: the need and desire of congregants to gather, the rate of COVID-19 infection in the community, and the risk of COVID-19 infection and complications among the church’s congregants. I created three figures to describe how these factors of churches gathering influence three vaccination periods:
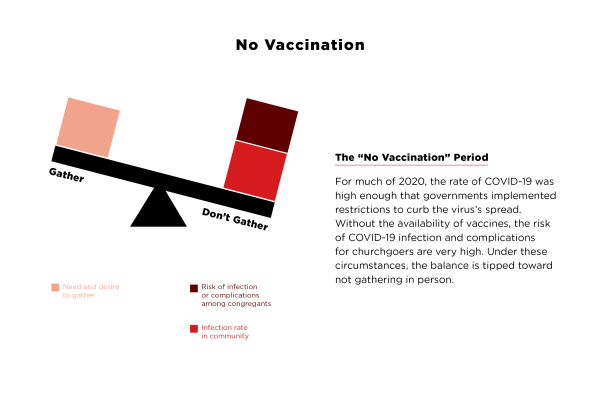 Figure by Mallory Rentsch / Data Compiled by Daniel Chin
Figure by Mallory Rentsch / Data Compiled by Daniel Chin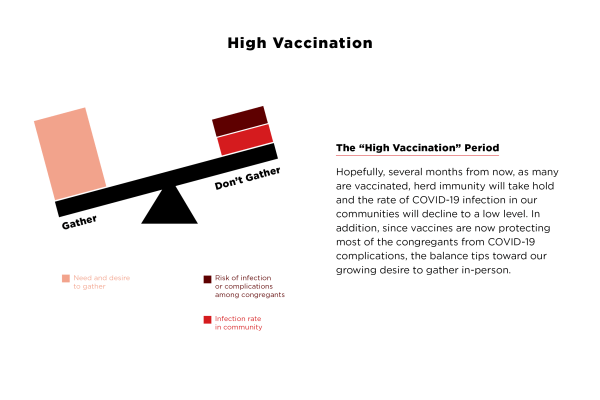 Figure by Mallory Rentsch / Data Compiled by Daniel Chin
Figure by Mallory Rentsch / Data Compiled by Daniel Chin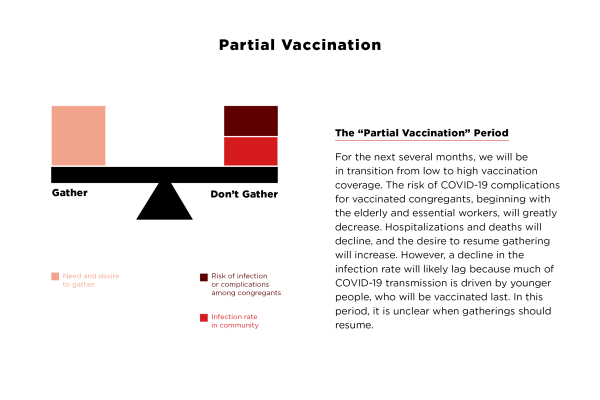 Figure by Mallory Rentsch / Data Compiled by Daniel Chin
Figure by Mallory Rentsch / Data Compiled by Daniel ChinThe partial-vaccination period will last until there is herd immunity against COVID-19 and the infection rate declines to a low level. How long this takes is affected by the availability, effectiveness, and uptake of COVID-19 vaccines as well as the contagiousness of new COVID-19 variants. The media will report on these issues in the months ahead, and church plans may need to adjust as new information becomes available. However, here is background on two important issues.
First, scientists are still unsure about whether vaccinated individuals who are not apparently ill from COVID-19 can harbor the virus and spread it to others. Recently approved vaccines can reduce the risk of COVID-19 illness by more than 90 percent, including the virus’s serious complications. But if the virus can spread through the vaccinated, then we must continue to use masking, physical distancing, and other means to protect vaccinated individuals from COVID-19 in the same way we protect unvaccinated individuals. The purpose of this, however, would not be to prevent COVID-19 complications but to limit the spread of the virus.
Second, fast-spreading variants of COVID-19 in different parts of the world appear to be 10–70 percent more transmissible. This is an alarming development because these variants may worsen and prolong the pandemic. Fortunately, most scientists believe current COVID-19 vaccines should remain effective against these variants.
Since the spread of these COVID-19 variants could delay the time to reach herd immunity, the need for our churches to have plans on how and when to gather is greater than ever. If these virus variants become more common in our communities as anticipated, then we need the suggestions below even more to minimize the spread of COVID-19 in our churches. Because COVID-19 and all its variants spread through nasal secretions and respiratory droplets, the ways to contain their transmission remain the same. Therefore, my suggestions remain relevant even with the spread of these variants.
Five suggestions for a gathering plan during the partial-vaccination period
1. Use the level of COVID-19 infection as the primary guide for congregational gatherings.
If in-person gathering resumes during this period, vaccinated and unvaccinated attendees will mix with each other. Because herd immunity has not been achieved, COVID-19 infection rates in our communities will remain high. Given that our church activities facilitate virus spread, there is still a high risk of transmission between the unvaccinated and even between unvaccinated and vaccinated congregants. If scientists determine that vaccinated individuals can still harbor the virus and spread it, then even after a high proportion of people are vaccinated, the risk of spread may remain high as long as the level of COVID-19 infection in the community remains high (see upper figure). Only when the infection rate declines to a lower level will the risk of transmission between congregants also decline and then in-person gatherings can safely resume (see lower figure).
Therefore, this partial-vaccination period is an especially tricky time because the risk of COVID-19 complications for unvaccinated congregants has not decreased, but the desire to gather will likely increase. This will undoubtedly influence a church’s decision to gather. Therefore, the decision on when it is safe for vaccinated and unvaccinated congregants to gather should primarily be based on the level of COVID-19 infection in the community and not on the proportion of congregants vaccinated.
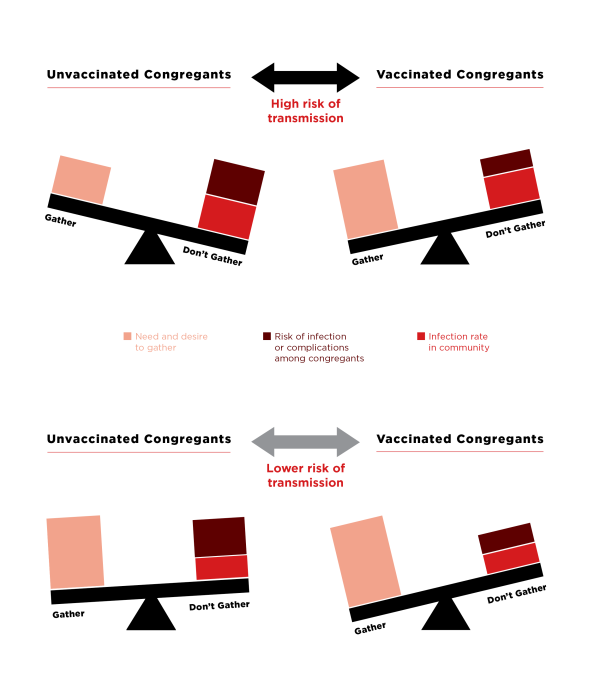 Figure by Mallory Rentsch / Data Compiled by Daniel Chin
Figure by Mallory Rentsch / Data Compiled by Daniel Chin2. Consider allowing vaccinated congregants to gather separately.
Although churches may choose to gather only when both vaccinated and unvaccinated congregants can mix safely together, there is an option to gather earlier with just vaccinated congregants. Because vaccinated congregants are protected from serious COVID-19 complications, it is much safer for them to gather indoors even when the infection rate in the community is high. Many of our elderly and more vulnerable church members, who will be vaccinated earlier, may welcome an earlier opportunity to gather before everyone can safely do so. An easy first step would be small groups for vaccinated individuals.
However, church leaders may have reservations about separating their congregants into groups. Laurie Brenner, a pastor of a Seattle neighborhood church deeply engaged in the community, said, “In my medium-size church, there is a real tension. On one hand we do not want to separate people; on the other hand people want to meet as soon as possible.”
But the church leaders I talked with generally believe it is possible to set up gatherings just for those who have been vaccinated. Broughton said, “Pods are already popping up spontaneously that bring people with lower risk for COVID-19 together. These are being self-managed by the members themselves. I can see the same with vaccinated members.” Brenner added, “We need to work to ensure that vaccination does not end up dividing existing groups.”
In general, the idea of a parallel structure for both vaccinated and unvaccinated congregants seems to resonate with these leaders. George Hinman, the senior pastor of the large multigenerational church that I attend, said, “I can accept the idea of having a worship service just for the vaccinated if we also provide another option for people to worship regardless of their vaccination status. We need to give everyone an accessible experience.”
Nevertheless, limiting gatherings to only vaccinated congregants could prove challenging as churches may be reluctant to require a proof of vaccination for entry through their doors. However, the idea isn’t new; the use of health passes could become commonplace in the coming months.
3. Take a step-wise approach to resume specific forms of in-person gathering.
We need a step-wise plan because different church activities have different risks of COVID-19 transmission. Activities that carry a higher risk of airborne COVID-19 transmission should start only when infection rate is low, while those with a lower risk can start at a higher infection rate. Moreover, it is easier to mitigate COVID-19 transmission in some activities compared to others.
The table below provides guidance on in-person activities that can start once the level of COVID-19 infection drops to certain thresholds. It builds on the step-wise plan for church reopening that I wrote in an earlier CT article and provides thresholds of infection for the steps. For those who live in the US, the tricky part is that there is no national standard for high or low levels of infection, though health departments have come up with similar thresholds of infection for their use. I have adapted them for the steps in the table.
One confusing aspect is that COVID-19 case rates are sometimes presented as the total number of cases over 7 or 14 days per 100,000 residents instead of the daily number of cases per 100,000 residents. In the table, I recommend using the daily number as thresholds, so you may have to convert your local health department’s number to use the table or use a global dashboard with this information, such as the one by STAT News. Always keep in mind that insufficient COVID-19 testing may underestimate the true infection rate; therefore, in communities with inadequate testing, be more conservative in starting activities.
As more information becomes available or clearer guidelines emerge, the thresholds in the table may need to be adjusted. Churches may choose slightly higher or lower thresholds for starting activities. With the fast-spreading variants, it is even more important to start activities at each threshold with a smaller number of individuals. Given that infection rates have skyrocketed in the last few months in many areas, it will be a while before infection rates decline to a level that will permit indoor gatherings for unvaccinated congregants.
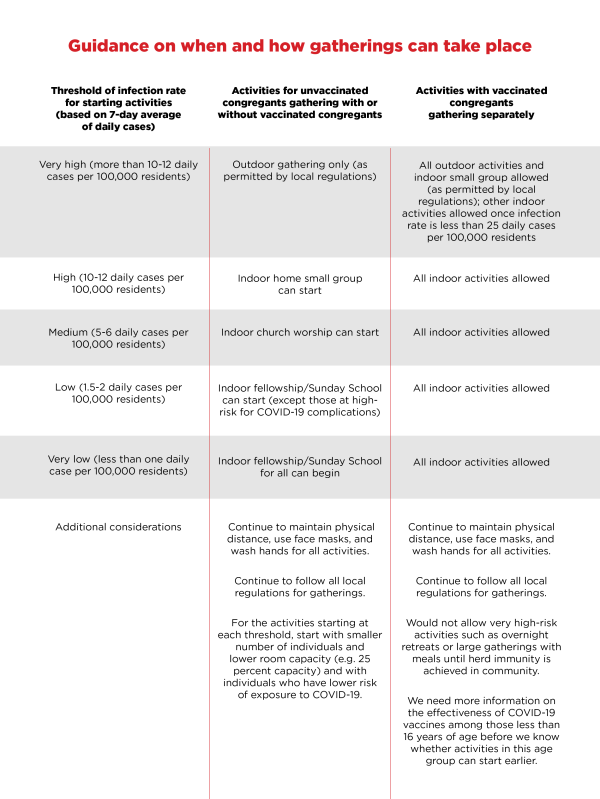 Table by Mallory Rentsch / Data Compiled by Daniel Chin
Table by Mallory Rentsch / Data Compiled by Daniel Chin4. Encourage congregants to reduce their risk of exposure to COVID-19.
As COVID-19 vaccines are rolled out, many churchgoers are in a lower priority group for vaccination, and some may never be vaccinated either by choice or due to health reasons. Regardless of the reason, it is important for unvaccinated congregants everywhere to be able to gather safely with others in their churches.
Disease control experts have long recognized the importance of behavioral change in helping people reduce their risk of exposure to an infectious agent. Before our church attendees gather, we can ask them to modify their behaviors to reduce their risk of exposure to the COVID-19.
The risk of exposure to the virus is simply sharing the air that other people breathe. Our congregants can lower this risk by reducing their close contact with others (defined as being within six feet of another person for at least 15 minutes) and increasing the use of face masks, physical distancing, and well-ventilated spaces when meeting with others.
When we gather with others in our churches, we can love our brothers and sisters by protecting them from the harm of this virus. “It is fair to ask people to mitigate their risk for the sake of others. I believe it is even fair to ask for vaccination before gathering. But it is important not to exclude people. We need to provide options for all,” said Hinman.
“Our church emphasizes the importance of personal accountability and not just what the church mandates,” said Elton Lee, an elder of a large Chinese American church, who is grateful for members who take responsibility to protect others. “The church can provide guidelines, but it is up to individuals to adhere to them.”
To help our congregants take responsibility, it would be helpful if they knew their risk level. A few apps are designed to help individuals estimate their risk of catching COVID-19 at a gathering. But with COVIDRisk.Link, a tool I recently developed with others, congregants can monitor their own risk of exposure to the virus on a regular basis and reduce their risk, if necessary, before meeting with others. The spread of the new virus variants, which increase the contagiousness of individuals with COVID-19, makes this more important. In addition, the use of this assessment tool can help congregants form social bubbles to meet more safely with those who have a risk of exposure with which they are comfortable.
At every threshold of infection in the above table, gatherings can be safer if we ask congregants to reduce their risk of exposure to the virus, and we encourage those with a lower risk of exposure to participate in activities sooner than those with a higher risk.
5. Encourage your congregants to get vaccinated.
If a significant proportion of people in our communities refuse to be vaccinated, this will prolong the pandemic and its harmful effects on our society. Unfortunately, nearly 40 percent of Americans and a slightly higher percentage in American churches are reluctant to be vaccinated. Broughton explained, “Our people are currently reacting based on fear because of the influence of past experiences like the Tuskegee experiments. They don’t know if they can trust the vaccines.”
Because we know that COVID-19 vaccines can protect people from the harmful effects of this virus and allow us to return to normal church ministries sooner, in my opinion, churches should be promoting COVID-19 vaccination. Not only will vaccinated Christians be protected from serious complications if they get infected, but they will also be able to serve others in need sooner and contribute to ending the pandemic.
It is unfortunate that this pandemic has been so politicized that some church leaders are hesitant to endorse vaccination, but I suggest that we use the Great Commandment as our primary motivation. Although experts are not certain vaccination will prevent the spread of COVID-19, there is a very good chance that vaccines will reduce at least some (if not most) COVID-19 transmission. Therefore, let us love one another by encouraging vaccination, especially those in our churches.
But it may take significant efforts and patience to communicate with our church attendees about the benefits of the vaccines. Broughton emphasized this, “I need to continue to have conversations with the congregation. Where this information is coming from makes a big difference to them. The trust greatly increases when they know it is coming from men and women of faith who are knowledgeable about science.”
More important than words are actions. Church leaders can set an example to their congregations by getting vaccinated themselves. There is a lot of distrust of the government, of science, and of COVID-19 vaccines. The most trusted members of many communities are in our churches. Therefore, church leaders can play an important role in encouraging their congregants to get vaccinated.
With the start of COVID-19 vaccination in our communities, we are beginning the long road back toward normalcy. At the same time, the US is experiencing the most tumultuous and divisive period in its recent history. Hinman said, “As the church, we cannot allow how we handle this pandemic and the issue of vaccination to divide us.” To help our churches move forward in unity, I pray these five science-based suggestions can help our churches to be a beacon of light—embracing faith and science—as we resume gathering and continue serving the world around us.
Daniel Chin is a physician trained in pulmonary and critical care medicine and epidemiology with 25 years of global public health experience. In 2003, he led much of WHO’s support to China to contain the SARS epidemic.